Prof. Dr. Alberto Lifshitz, a recognized Mexican medical educator, "shares the view that diagnosis by analogy, which is the most often taught, is insufficient." In his opinion, what Practicum Script does while breaking with traditional formats of single correct answers and confronting uncertainty, "is not a very well understood subject by hard scientists, but it is the scenario in which we, clinicians, move."
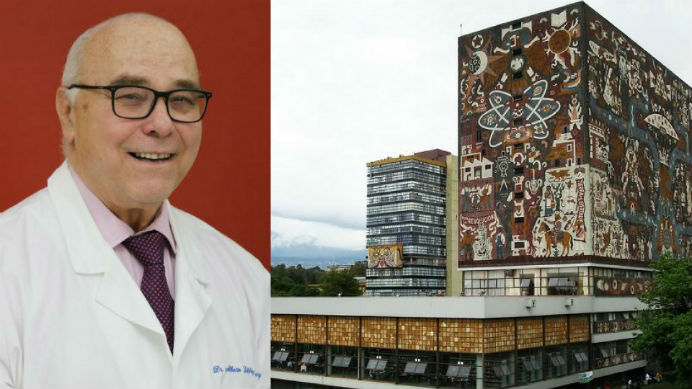
City of Mexico - July 26, 2018. Alberto Lifshitz is a surgeon, graduated from the Autonomous University of Mexico (UNAM), and a specialist in Internal Medicine by the Mexican Institute of Social Security (IMSS). Within UNAM, Dr. Lifshitz has worked since 1972 in the School of Medicine as a professor and Secretary of Clinical Teaching. In addition, he has been a Head of Department, Head of Division, and Director of the Hospital of Specialties of the Medical Center of IMSS, as well as a coordinator of Medical Education in the same institution. Likewise, he has been the Head of the Education, Research and Health Policy Unit of the IMSS and Secretary of the General Health Council until 2012. Endorsed by years of experience and positions of special relevance in his country, he talks about the “new clinic" associated with the 21st century.
You have been a professor of undergraduate and specialization courses in medicine, synod of the practical phase of the professional examination of the medical career at the Faculty of Medicine of UNAM, and director of thesis for obtainment of the degree of specialist. What future do you predict for the profession?
As it responds to continuous and renewed social needs, the profession will have to follow its mission, but obviously, it will change depending on a series of transformations, both scientific and technological, conceptual, social, methodological. Medicine is already different compared with classical medicine because of all these influences.
How does this break with the classical mechanistic and rationalist paradigm?
I am not an expert, but I understand that complexity refers to the large number of variables that participate in a certain phenomenon, which are interconnected in a network, and that any change in any of them affects the whole. In medicine, one can no longer speak of "the cause" of the disease, since all diseases are multicausal and even have the participation of subjective elements.
Would you say that we have to shift the focus from teaching to learning? How?
Of course. The important thing is not what the professors do but what happens with the students. Only learning legitimizes the educational act. It is necessary to verify it (that is what assessments are for), but also if the competencies acquired are expressed in the performance and if this has an impact. We must encourage professors to moderate their arrogance and think about the consequences of their actions.
Recently, the Practicum Foundation attended a meeting that listed three challenges in the field of Medical Education: orphan competencies, new technologies, and teaching by clinical tasks. Do you agree with this vision of things?
If by orphan competencies we understand the transversal ones, I share the idea of their hierarchy. Students, regardless of their disciplinary orientation and individual interests, have to achieve these competencies. The new technologies, of course, offer a range of alternatives, both educational and clinical, once unthinkable; the key is to approach them critically, obtaining the maximum benefit from them but without being subordinated or enslaved. Clinical tasks are the foundation of learning and the paths to expertise in the area.
What is your opinion about simulation? Beyond the training of psychomotor skills, to what extent is clinical reasoning training beneficial?
The use of artificial patients (mannequins, standardized, electronic) certainly helps to mechanize some skills, but sooner or later, the students have to face real patients. Only facing them, they do learn certain contents such as empathy, compassion, doctor-patient relationship, or solidarity.
How do you assess, in particular, the real clinical cases simulator Practicum Script?
I like it very much. I believe that structuring diagnostic and therapeutic thinking (and even prognostic thinking) is still an unsolved pedagogical need in many schools. I also like the denomination of "clinical thinkers" that hierarchizes this activity. I share the view that diagnosis by analogy (how close are ailment and illnesses?), which is the most often taught, is insufficient in many cases, as is an exhaustive vision such as searching for everything to see if something comes out. Confronting uncertainty is not a topic very well understood by hard scientists, but it is the scenario in which we, clinicians, move.
When you were appointed Head of the Clinical Teaching Secretariat at UNAM in 2013, you were asked to implement the curriculum for competencies in clinical cycles. What happened with the challenge?
The plan was landed in clinical contexts, but I am not sure that it rests on the context of the competencies. Not all of our professors had understood it and they have long inertia. With the academic progress exams, we will be able to know if the plan for competencies landed well.
Are iatrogenesis, use and abuse of technology, and lack of personal interest in the patient taboo subjects?
Historically, they are taboo subjects, but recently they are spoken of with greater openness. They are topics of extraordinary importance for the contemporary practice of the profession and must be approached from a self-critical and proactive perspective. It has also been a taboo to talk about physicians’ rights, their mistakes and the demands of society, but they are increasingly being addressed with greater maturity.
You have published more than 270 articles in medical journals. What value do you give to research?
Without a doubt, it has been the path of progress in clinical practice (and in other disciplines of medicine). All students should have exposure to research, not always so that they become original researchers themselves, but to be trained in certain very important contents for the professional practice: careful observation, questioning, theoretical deepening, systematization or order, among others.
Our personalized help center enables you to obtain technical support and help for navigating through the site and using the program.